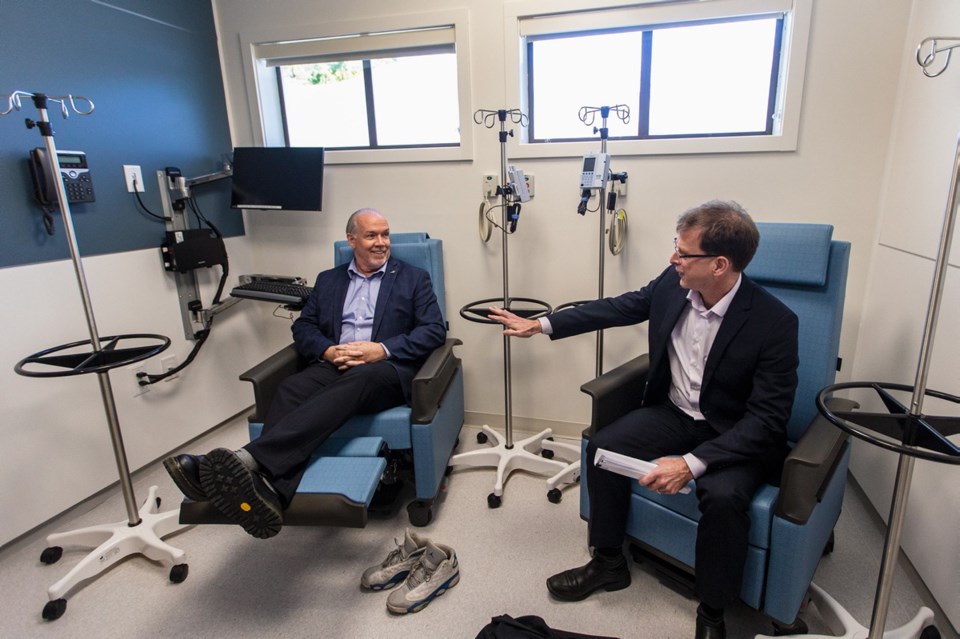
More than 25,000 patients visited the urgent primary care centre in the West Shore in its first year, says B.C. Health Minister Adrian Dix.
“In terms of patient visits, it’s the most popular, the most-used urgent primary care centre in B.C.,” Dix said of the clinic, which opened on Nov. 5, 2018. “It’s leading Surrey. It’s leading Vancouver. It’s leading similar high-population areas.”
The clinic, one of 14 in the province, is also home to the CARES mental-health clinic, which has handled more than 500 counselling visits since opening in February. “I think it shows both the significant demand in the area, the need for the service of an urgent primary care centre and the success of the centre,” Dix said. “I think it shows how effective team-based care is.”
About 19 per cent of West Shore residents don’t have a family doctor. The provincial average is 17 per cent.
The provincial government began opening urgent primary care centres in 2018. They are meant to provide same-day access for people with non-emergency illnesses and injuries who need to be seen within 12 to 24 hours, relieving pressure on hospital emergency rooms.
They also try to “attach” patients to family doctors at the centre or in the community and offer patients ongoing care through appointments with doctors and nurse practitioners.
The Westshore Urgent Primary Care Centre in St. Anthony’s Medical Centre on Goldstream Avenue in Langford employs a staff of 84 and is open from 8 a.m. to 8 p.m., seven days a week.
The medical centre also offers a laboratory, medical imaging, a pharmacy and space for family doctors’ offices.
The urgent care centre saw about 1,100 patients in a two-week period in October, or about 78 patients a day, according to the Health Ministry. Fifty-nine per cent of patients seen in its first year of operation did not have a family doctor.
Annual staffing and operating costs are about $4.45 million for more than 28 full-time-equivalent positions. A one-time startup cost of $36,000 was also provided. The capital costs are estimated to be $4.25 million, 30 per cent of which is expected to come from the Capital Regional Hospital District.
Doctors who have criticized the urgent primary care centre model argue physicians in private practice treat more patients at less cost and provide long-term care. Family physician Dr. Steven Keeler worked at the original St. Anthony’s medical treatment centre, run by about 15 family doctors, for 25 years. He now works in View Royal and periodically at the Westshore Urgent Primary Care Centre.
At his View Royal office, three doctors see about the same number of patients each day at less cost to the government, he said. They have a patient roster of about 4,000, seeing about 80 patients a day. Physician income is about $700,000 annually.
Of that, about $200,000 is spent on overhead, which includes three staff, according to the practice.
The urgent-care centre has excellent clinicians and staff and provides good-quality care, but it’s not connecting patients with family doctors, Keeler said. “While they are providing access — which is no different than the current clinics in the area — they are not attaching the 40,000 unattached patients to better longitudinal care provided by family physicians.”
Dix concedes the number of patients who have connected with a family doctor through the West Shore clinic is lower than expected, at about 300 patients. In Kamloops, for example, a centre using a slightly different model has attached thousands to doctors, he said.
“Our goal in the second year is to build out attachment through primary-care networks in the area,” Dix said. “In that area in the West Shore, there’s significant need and this responds to part of that need. It’s not the whole solution, and I’m not suggesting it is.”
Of the visits to the West Shore centre, 69 per cent were for less urgent cases (hypertension or a urinary tract infection, for example) and 11 per cent were for non-urgent cases (minor cuts or wounds, for example).
That shows “the public understands the value and the need for the primary urgent care centre,” said Dix.
In 2017-2018, 29 per cent of all Victoria General Hospital emergency visits were for non- and less-urgent cases, according to the Health Ministry, citing data from Island Health.