Vancouver Island has the second-highest number of fentanyl-related illicit-drug overdose deaths among health regions in the province, according to a coroner’s report released Thursday.
Victoria is in the top three municipalities for overdose deaths since 2007, alongside Vancouver and Surrey.
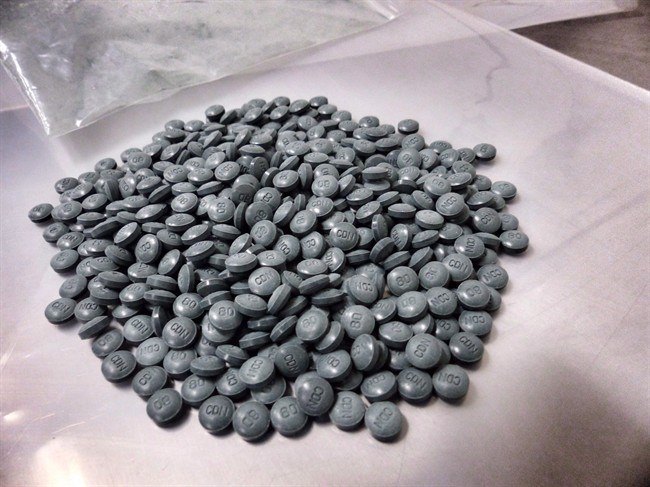
Nanaimo is in the top three municipalities for fentanyl-detected overdose deaths, also alongside Vancouver and Surrey. Fentanyl is a highly toxic synthetic opiate used in prescription drugs that is being cut into illicit drugs such as heroin and cocaine.
“There has been a surge of overdose deaths here, more than our fair share,” said Dr. Paul Hasselback, Island Health’s chief medical officer for central Vancouver Island.
According to the report, 433 people in B.C. have died from drug overdoses from January to July of this year.
That averages about two deaths per day and is a 74 per cent increase from 2015. Two-thirds of the deaths were fentanyl-related.
In seven months this year, 34 people in Victoria have died from illicit-drug overdoses.
There were 17 deaths in all of 2015.
“We’ve been so concerned, we put in an emergency-response plan in January,” said Hasselback.
He said it is not just deaths Island Health and other agencies are concerned about. Overdose visits to hospital have also nearly doubled.
“Mostly driven by Nanaimo Regional and Royal Jubilee [hospitals],” Hasselback said, noting: “Most fatalities occur outside of the hospital.”
Hasselback said the cause of the overdose increases is hard to pinpoint, but is “likely related to the innovation and distribution of the illicit-drug network.”
He said Island Health is part of prevention groups collecting data and increasing access to naloxone — a life-saving antidote to the fatal effects of heroin and fentanyl — for first responders, agencies and users.
“The kits are predominantly dispersed to the user community. They are often the first responders,” he said, adding that engaging users and improving access to safer consumption sites and addiction medication would likely have the greatest impact.
Mark Wilson, a co-ordinator at the Society of Living Illicit Drug Users, said the overdose statistics are further proof that Victoria needs a supervised safe-injection site.
“The sad part is we’ve been saying it all along,” Wilson said. “The awareness is already there, but people will use.”
Wilson said there is progress with the availability of naloxone. Everyone on his team of 15 volunteers has used a kit to help save a life.
Outreach workers, including current and former drug users, are on the streets daily.
“They’re trained to use the kits, but not as nurses. It’s putting them on the front lines in a stressful situation,” Wilson said. “Focusing on the drugs or where they come from won’t make the difference. We need to focus on the safety of users.”
Provincial health officer Dr. Perry Kendall, who declared the rise in overdoses a public-health emergency in April, said overall the fatality numbers appear to be “plateauing” instead of decreasing.
“It’s disappointing, but I don’t think these things get turned around overnight,” he said. “So if we’re seeing this stabilizing rather than an ongoing increase, that is perhaps a reason for optimism.
“We hope and would very much like to see the numbers start to come down in future months.”
Kendall said he’s hoping to see the fatality statistics begin to trend downward before the end of the year.
Kendall, who co-chairs a task force dealing with the issue, said getting more information to the public about the risks will make a difference.
For instance, some deaths involved people using drugs alone, so that nobody else was available to call 911 or administer naloxone.
“If we could get people — if they have to use — to use more cautiously, always have somebody present. That would help, because then we can reverse an overdose.”
Kendall said getting more people into substitution treatment, such as methadone, or making such treatment more available also will be key.
He said health officials, researchers, police, first responders and the coroners service are working closely to deal with the issue.
“We’re working so that we can be sure that people will not be scared to call 911,” Kendall said.
“In the past, I know, they’ve been worried that if the police come, they’ll be hassled or harassed. So where police are first responders, we’re trying to get the policy changed so that they’re there primarily to save lives.”
In light of the coroner’s report, the provincial government said it would expand the naloxone program and work to make nasal-spray kits available in B.C., as well as work with the federal government to establish supervised consumption sites, restrict pill presses and access to drug-making materials, enhance trafficking charges and set up a fentanyl-testing service.