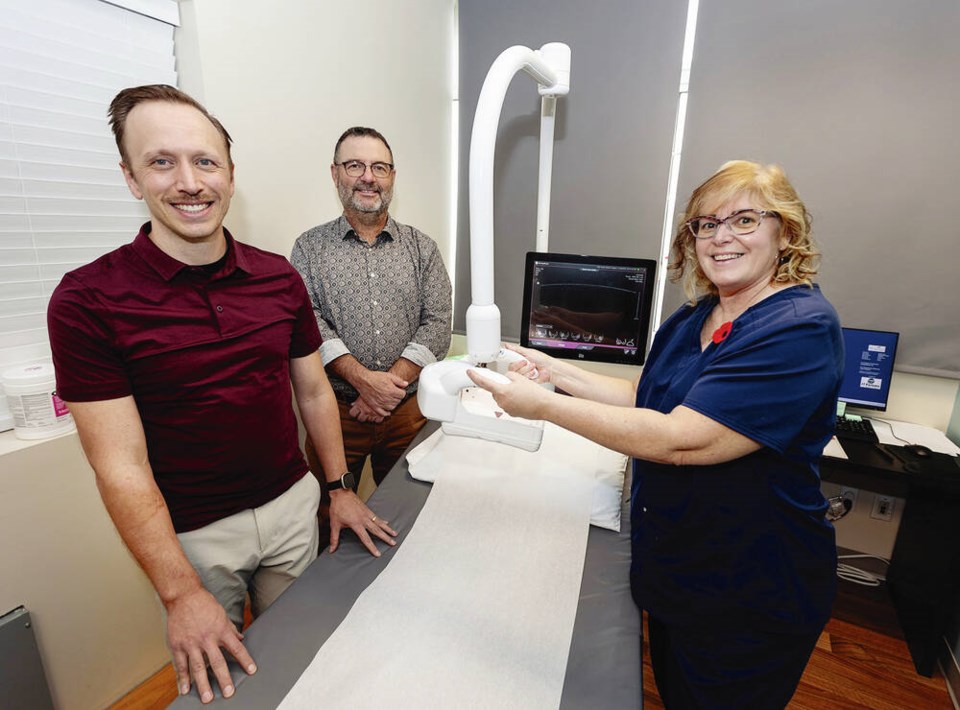
A Victoria clinic offering dense-breast ultrasound screening says its newest automated machine — one of the first in the province — can scan five times the patients its handhold probe can manage in a day.
Regional manager Allen Lavoie said the automated breast-imaging ultrasound machine at West Coast Medical Imaging on Fort Street scans about 16 women a day, compared with about three a day with its “fairly demanding” traditional handheld ultrasound.
“This technology — automated breast ultrasound — is offered throughout Canada and the United States but we have not had it offered anywhere in British Columbia until now,” said Lavoie. “To our knowledge it is the first.”
In B.C., routine mammograms have been offered since 1988. In 2018, B.C. became the first province to also provide a breast-density rating with mammogram results, and the next year it offered publicly funded supplemental ultrasound for people in the highest breast-density range.
Individuals with dense breasts are at increased risk for breast cancer and have a higher probability of an invasive breast-cancer diagnosis in the two years following a screening mammogram, according to B.C. Cancer.
The higher the dense breast BI-RADS rating — A, B, C, through D — the more likely that a mammogram could miss a small tumour, given that both the tumour and dense tissue appear as white on high-resolution digital X-ray scans. Fat appears black.
West Coast Medical Imaging says it receives referrals for the bulk of Island patients for breast-screening ultrasound, which uses high-frequency sound waves to create an image.
Until now at the Fort Street clinic, screening has been done by a handheld ultrasound probe. In an ideal world, all screening would be done this way, Lavoie said, but it’s time-consuming — about 45 minutes per patient — and physically intensive, allowing only a few a day to be performed by sonographers, of which there is a shortage.
Since having the automated machine, the Fort Street clinic has cleared a backlog “of several hundred” patients in about four months, said Lavoie, a technologist.
“We are caught up with screening breast ultrasound and going forward, we want to offer this to physicians that wish to co-ordinate mammograms with breast ultrasound screening for women with dense breasts,” said Lavoie. “Now we can book them when people want them performed.”
Dr. Stuart Silver, a radiologist and medical director at West Coast Medical Imaging who also works at Royal Jubilee Hospital, said the breast-cancer detection rate for the automated breast ultrasound is similar to the handheld device, and if more women can be scanned faster with the automated machine, more cancers can be caught earlier.
“We’ve only been doing it since August — somewhere between 500 and 600 scans — and we’ve found three or four small cancers completely missed at mammography,” said Silver. “We’re able in those cases to change that woman’s prognosis considerably because we’re finding tumours when they’re small.”
An estimated 28,600 women will be diagnosed with breast cancer every year in Canada, and 5,500 women will die from it. It’s the most common form of cancer in those born female in Canada and the second leading cause of cancer deaths, according to the Canadian Medical Association Journal last year.
Silver said the same tumour caught by the automated ultrasound in dense breast tissue may not show up in mammography even two years later.
“They probably wouldn’t find it until they could feel a lump and by the time you can feel a breast cancer, it’s getting big,” said Silver, “it’s getting to a size where you’re worried that there’s going to be metastases to the lymph nodes in the armpit and maybe even further away, and the chance to treat successfully goes down as the size of the tumour gets big.”
The Canadian Cancer Society says while research shows breast ultrasound or an MRI might find additional cancers in women with dense breasts, these tests can have a high rate of false-positive results, and there isn’t enough evidence yet to recommend other tests beyond mammogram for women based only on their breast density. Lavoie said the technology is improving all the time.
Radiologist Dr. Paula Gordon, a clinical professor in the department of radiology at the University of British Columbia, said in a peer-reviewed paper in the B.C. Medical Journal in May that women with dense breasts should have supplemental screening with ultrasound, MRI, or other emerging technologies.
“Women with dense breast tissue deserve the same opportunity for early detection of breast cancer as women with non-dense breasts,” she wrote. “They should be encouraged to have supplemental screening, usually with ultrasound.”
As with mammography, women should be informed, in advance, that false alarms with ultrasounds are common as they are in all screening tests, said Gordon in an email.
“Women experience anxiety if they are called to come back for more tests, but it’s short-lived,” said Gordon. “It is not a reason to deny women screening, because then we lose the opportunity to find the potentially lethal cancers.”
>>> To comment on this article, write a letter to the editor: [email protected]