At the end of his testimony Dr. David Harrison left the witness box at a coroner’s inquest on Thursday and embraced father Brock Eurchuk. The two men openly sobbed, bringing the proceedings to a standstill.
Mother Rachel Staples, recovering from surgery, wept and rose from her wheelchair to join the embrace.
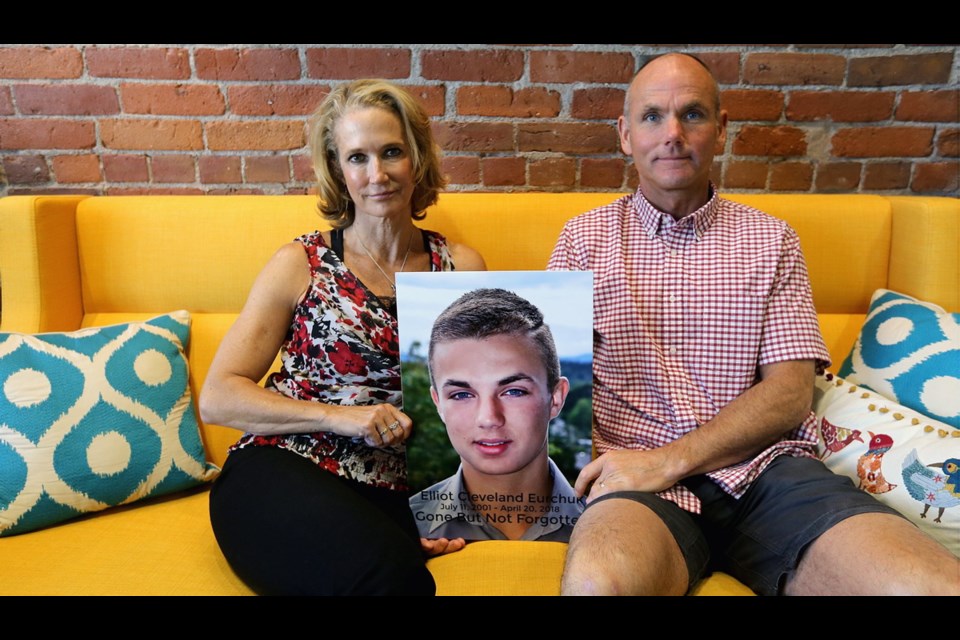
It was another emotional day of testimony into the April 20, 2018, drug-overdose death of Elliot Eurchuk, 16, of Oak Bay. Five jurors are tasked with making recommendations.
Harrison testified about his moral and legal struggle over releasing drug-test results to Elliot’s parents just months before the teen died.
“Internally I was struggling — should I share and disclose information to the parents,” said Harrison.
“On one hand, Elliot has rights to his information not being shared if he chooses or elects not to share,” said Harrison. Elliot had asked that his information remain confidential. “On the other hand, there was a life at risk to the point I didn’t think he was making good judgments. He didn’t have the capacity of decision making. … It was a hard decision to make.”
Staples had begged for the drug tests to convince her husband of what she had already suspected: Their son was dependent on street drugs. Given their son’s denials, Eurchuk needed scientific proof .
Harrison said of the B.C. Infants Act: “The legislation is very hazy. It needs to be clarified: When is it in the best interest of the child to disclose information.”
Island Health’s interpretation of the legislation, said Harrison, is that if a child 12 or older doesn’t want their medical record released, it can’t be.
Harrison testified there is a lack of services for mental-health issues and for adolescents dealing with addiction.
In addition to more services, he recommended a mental-health and addictions nurse to guide adolescents and their families once discharged from hospital until they are enrolled in services.
Harrison said he saw Elliot on Feb. 16, 2018 after the teen overdosed in Victoria General Hospital, where he was admitted that month for a blood infection.
After talking to Elliot, Harrison felt that his patient did not understand the consequences of his actions. “In that conversation, I didn’t get a good sense that he had capacity in terms of the gravity of the situation,” said Harrison. “I did lay out, it was a serious event. He could have died.”
Staples has said that on Feb. 16, 2018, Harrison left her in his office with Elliot’s hospital drug-test results left open on his desk. The lab test confirmed Elliot overdosed in hospital on Feb. 10, 2018, and he had cocaine and fentanyl in his system.
Several physicians testified about problems with the B.C. Infants Act.
The legislation allows a child confidentiality so that doctors can help in situations involving abuse, sexual abuse or abortion — issues a child might safely disclose only in confidence. However, the confidence can also allow a child to hide issues from parents, including struggles with drug addiction.
Psychiatrist Dr. Mary Nixon said: “It’s always a balancing act between parents’ rights and individual rights and youths’ rights.”
Without access to a secure-care treatment facility where he could place his son involuntarily, his father phoned police with the hopes his son would be committed under the Mental Health Act and receive services that way.
Nixon testified that mental-health treatment is an individual thing. While involuntary secure-care admission for treatment for drug addiction — which is not her speciality — might work for some, it might not work for most others, she said.
“In terms of forced care,” said Nixon, “if you try to force anything it can cause someone to go even more underground than they are already.
“In Elliot’s case, we were already concerned with where he was at with his information sharing,” said Nixon. “It’s hard to say whether something like that would have made any difference for him or not.”
Nixon said attaining trust with a patient is key to helping them and that involves keeping their confidences unless they are in imminent danger of harming themselves or others.
After Thursday’s testimony, Staples spoke about the emotional exchange during the inquest. “My feeling is Dr. Harrison was extremely emotional after his testimony because he realizes there are significant gaps in our system, that had he been able to access those legally and provide us with the proper information and helped us, I think he felt he could make an impact helping Elliot survive and recover from what we now know was a substance-use disorder.
“I think he was emotional because he felt he was handicapped in helping Elliot achieve that.”