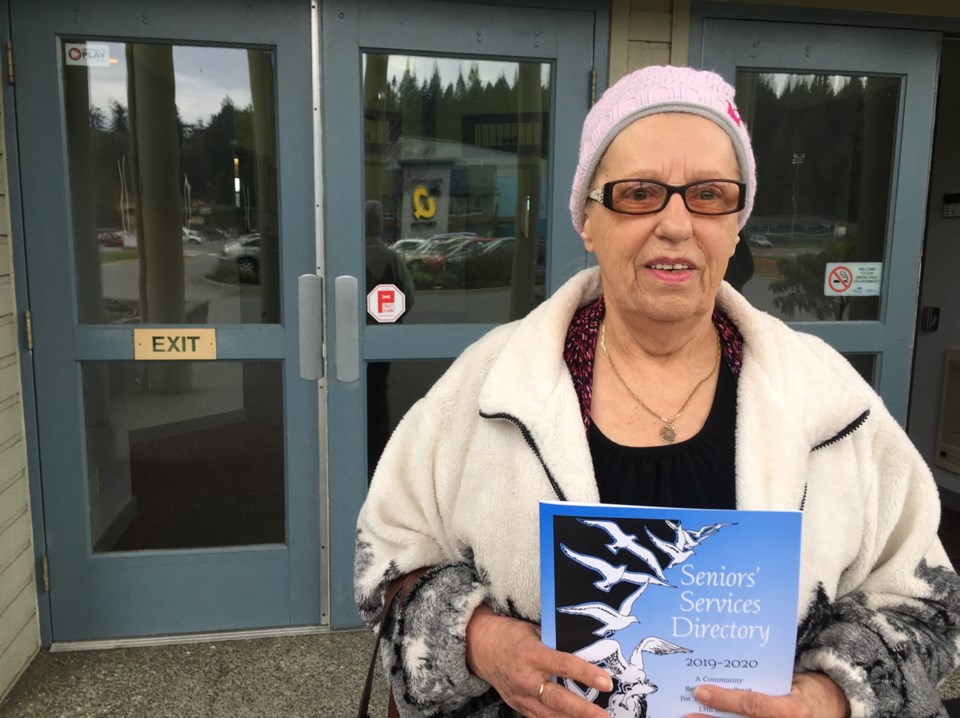
Senior citizen Pat Gordon says frustration over an hours-long wait for a prescription refill at the new Westshore Urgent Primary Care Centre caused her blood pressure to skyrocket.
“It’s really bad — there’s not enough doctors, there’s not enough staff,” said Gordon, who waited 41/2 hours to get a prescription for drugs for high blood pressure, high cholesterol and irregular thyroid. “When I finally got to see the doctor, my blood pressure was so high, he was really nervous about me,” said Gordon, speaking to Island Health’s board of directors at its public forum in Colwood on Thursday.
The urgent primary care centre in St. Anthony’s Medical Centre on Goldstream Avenue in Langford opened Nov. 5.
St. Anthony’s offers a laboratory, medical imaging and a pharmacy, and soon will house primary care practices.
The urgent primary care centre offers a team of physicians, nurse practitioners, nurses and mental-health and substance-use clinicians to treat episodic urgent cases — those that must be seen within 24 hours — as well as less-urgent health concerns for patients who do not have a family doctor or can’t see theirs.
The urgent care centre is part of a growing primary care network aimed at helping people who might otherwise go to a hospital.
In a presentation, Island Health talked about the successes of the $3.44-million centre — it will surpass 5,000 visits in the next week and is soon expected to double in capacity with the addition of another physician.
On the heels of that talk, however, Gordon gave the board members and executives a reality check, explaining how long she had waited.
“It’s terrible,” said Gordon, whose blood pressure had shot up to 169/90 by the time she saw a doctor. A normal blood-pressure reading is below 120/80.
Gordon said she has no family doctor, since hers retired last year.
Dr. Charlie Lamb, who was in the audience and asked to comment, called the situation a crisis.
“It is a crisis and the health authority and the ministry and the divisions of family practice do recognize it is a crisis and we need to do something yesterday about it,” he said.
“I want to reassure the public that we feel terrible as physicians to show up to those shifts … and see people with cancer, see people with diabetes, and know that they don’t have a GP,” said Lamb, a general physician.
Lamb has worked at other clinics, practices, urgent care centres and emergency departments and said all are experiencing the same challenges and need creative solutions and supports.
Marko Peljhan, Island Health executive director for urban Victoria, West Shore and Sooke, apologized for the length of time Gordon waited.
He said the health authority recognizes “there is a significant need in the community, so we are doing a lot of work to be able to address that.”
The clinic is one of 15 primary care networks to be created on Vancouver Island over the next three years. Health Minister Adrian Dix has said Nanaimo’s primary care centre is next, possibly to open March 31.
The West Shore clinic is open for same-day access 365 days a year.
Currently, the clinic is seeing about 50 patients a day and hopes to double that with the addition of a new doctor in the next few weeks, Peljhan said.
It is not nearly enough, he admitted.
“We will need many, many physicians to bridge the unattachment gap, the gap that we have in our community of folks who don’t have a family physician,” Peljhan said.
If Gordon had a family doctor, she would have had a booked appointment and not endured an unacceptable wait, he said.
“It’s really about establishing more practitioners in the community.
“We need to do so much more. We need to add services into the West Shore, into the St. Anthony’s professional centre, into all the primary care practices in the Western Communities and in Sooke.”
The solutions are multi-faceted, and the primary care centre in the West Shore is just a piece of that, Peljhan said, adding that divisions of family practice are working hard to recruit doctors into the West Shore clinics and to support established practices.
Gordon said she wanted to share her experience of the clinic-turned-primary-care-centre with Premier John Horgan.
“They can’t keep up and they are going crazy,” Gordon said.
Her experience speaks to a gap in services not only in the West Shore but throughout south Vancouver Island and other areas of the province, Peljhan said.
Gordon hasn’t yet tried to reach the premier because she imagines he was busy with allegations of extravagant overspending by suspended legislature clerk Craig James and sergeant-at-arms Gary Lenz.
“Doctors come out of medical school with about $260,000 in student loans,” Gordon said.
“That money they are wasting at the Parliament Buildings could have gone to educate these young people to go to medical school.
“Everything is screwed up around here.”