The provincial government has announced $5 million in funding to increase access to virtual mental-health services in response to the COVID-19 crisis.
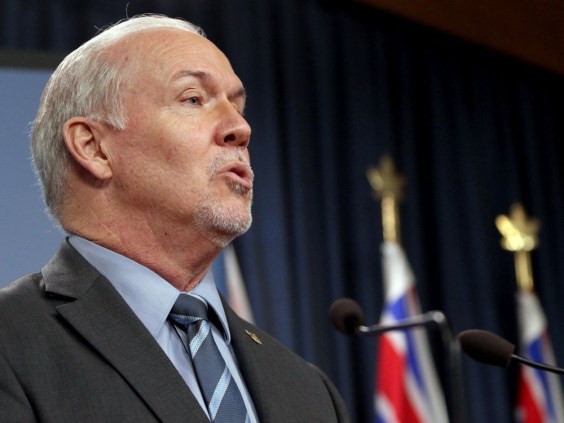
Premier John Horgan said that he knows the disruption to daily life has been hard on everyone, with many people feeling stressed, anxious, depressed or disconnected “from what the world was supposed to be.”
“We also need to step up and make sure that the COVID-19 pandemic is not going to adversely affect our mental wellness, whether it be through anxiety or depression or other stresses in what is now becoming our daily lives,” he said.
The funding announced will support mental-health organizations to expand existing programs and launch new services that people can access while they stay home to slow the spread of the virus. Among the expanded services are virtual individual and group counselling, mentoring programs and online courses for coping with stress.
The funding builds on a $10-million investment in the fall in community counselling agencies that provide no-cost or low-cost counselling.
Minister of Mental Health and Addictions Judy Darcy said the “overwhelming majority” of services provided through the new funding will also be free or low-cost. “Access to mental-health services in these unprecedented and difficult times does not depend on how much money you have in your bank account,” she said.
The funding will allow the B.C. branch of the Canadian Mental Health Association to support more than 3,000 additional people with increased access to existing programs.
CEO Jonny Morris said the association is anticipating a surge in need and the funding allows for early intervention.
“Some would describe loneliness as a significant public-health problem, and, as the premier said . . . it’s challenging to deal with isolation when we have to isolate physically,” Morris said, adding the association is grateful for the financial boost.
He said while much of the advice available suggests reaching out to others if you’re feeling down, that can be hard to do.
“We’ve been encouraging people to reach in, and so if you have people in your lives that might be alone right now . . . finding ways to reach in to vulnerable folks and connect with them virtually or by phone is really important,” he said.
The province has already increased support to seniors by providing a referral service to match volunteers willing to help with errands to seniors needing extra help.
CMHA’s Bounceback program for mental health is another avenue for seniors to access help over the phone.
Monique Sekhon, who runs a non-profit organization to connect people with mental-health resources and information, said it’s important to keep up with basic needs, such as eating healthy and getting exercise.
She suggests keeping a journal to process difficult feelings and express gratitude. “If that’s ‘I woke up today,’ that counts. Nothing is too small of an achievement,” she said. “You just need to be taking care of yourself.”
Sekhon, who has a degree in public health, said it’s particularly important for everyone, and especially people who live alone, to get outside while maintaining their physical distance from others.
“Getting outside where you can still see physically there are other human beings in the world and around you is a great way to remember that you’re not alone,” she said.
For those in mandatory self-isolation, that can mean just getting out in a private yard or balcony.
Another coping strategy Sekhon suggests is reaching out to offer support to others, whether it’s checking in on seniors who live nearby or friends you haven’t talked to in a while, or donating blood.
“And remember to turn it off. Close the computer. Put your phone away. Get away from screens,” she said.
The province is also expanding supports for front-line health care workers to help them cope with increased stress and safety fears at work.
A mobile-response team that normally provides support to workers on the front line of the overdose crisis will expand to include those handling COVID-19 emergency, with a specific focus on long-term-care workers.
About 200 psychologists have also volunteered their services for health-care workers, Darcy said.